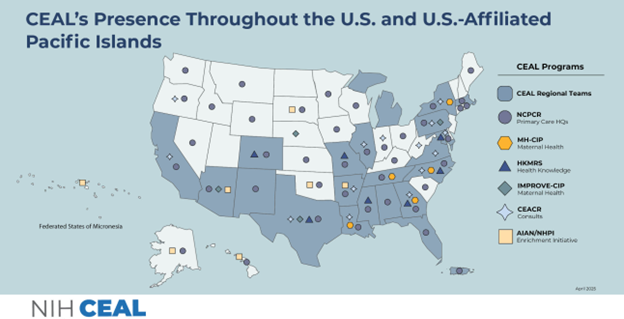
Morehouse School of Medicine is now part of a larger consortium of the CEAL Network for CEAL Network for Community-Engaged Primary Care Research (NCPCR) which will support the Community Engagement Alliance (CEAL) Against Social Determinants of Health (SDOH) and Chronic Disease (CD) Inconsistencies. This consortium includes an assorted ecosystem of partners and trusted leaders engaging in and working with communities across the country.

Topics
- Differences in Health Outcomes in Chronic Conditions
- Community-Specific Health Differences
- Primary Care Research
The Network for Community-Engaged Primary Care Research (NCPCR) aligns with the mission of the National Institute of Health’s Community Engagement Alliance (CEAL) program by using community-engaged research in primary care settings. NCPCR teams design and test interventions to address differences in health outcomes and improve participation in research.
NCPCR Components
The NCPCR program has two main components:
- A data ecosystem that uses the existing data warehouse capabilities and electronic health record data from primary care settings in CEAL communities, and
- A clinical trial conducted in the primary care setting. This component will show how the data ecosystem can encourage participation in clinical research and improve health care for communities with health challenges.
The data ecosystem will include information from community health centers (CHCs), which are geographically located in CEAL communities and provide primary care to patients often left out of clinical research opportunities.
The clinical trial will work with community health workers (CHWs) from CHCs to identify patients with uncontrolled diabetes mellitus or hypertension. These teams will also address challenges affecting patients’ ability to access regular health care or cope with chronic diseases, such as limited access to food, transportation, and jobs. CHWs can support patients by referring them to local social service organizations.
Educational materials such as fact sheets and brochures are available here.
 |
 |
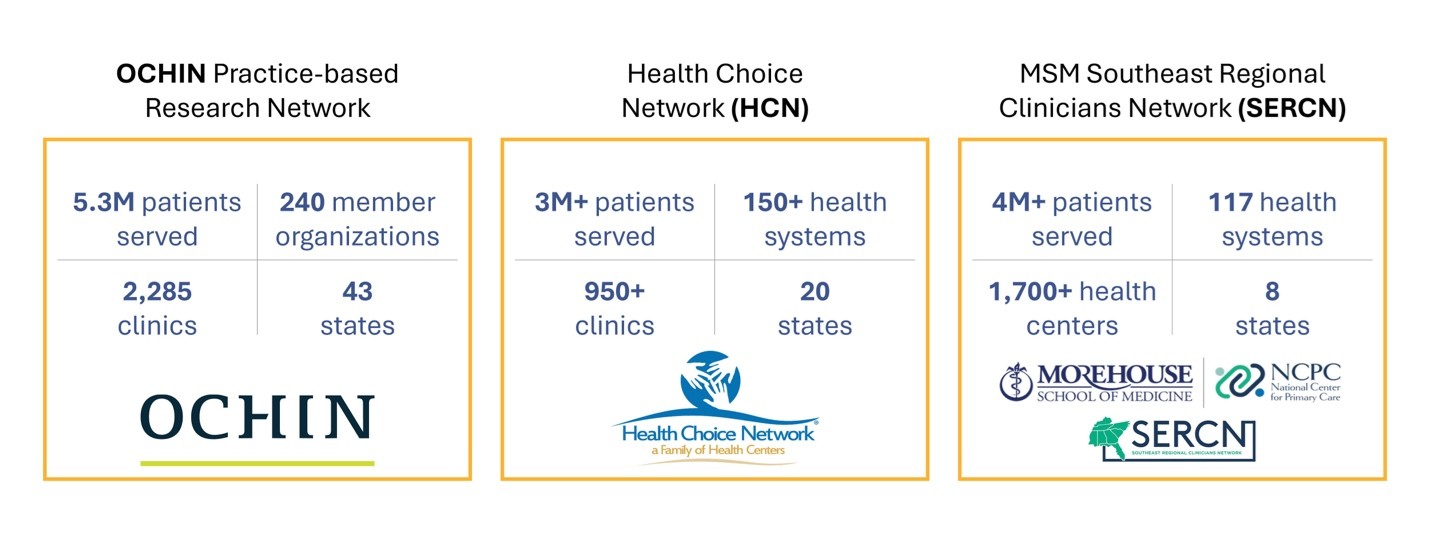
NCPCR Data Ecosystem & Clinical Trial Partners as of August 2024
Meet the NCPCR Team
Topic(s)
Steering Committee
Dominic Mack, M.D., M.B.A.
Dominic Mack currently serves as director of the Morehouse School of Medicine’s National Center for Primary Care (NCPC). A family physician, he is a longtime proponent of electronic health records. Under his leadership, the NCPC has several critical focus areas, including differences in health outcomes, access to care, and healthy lifestyle behaviors. His publications often focus on the topic of electronic health records and the role they play in advancing health. Dr. Mack joined MSM in 2001 and has served as medical director, and interim residency director for the Department of Family Medicine.
Angeloe Burch, Ph.D.
Angeloe Burch currently serves as the Chief Executive Officer for the African American Community Collaborative and the Executive Director for the African American Dance Ensemble. He is a Member of the NC Museum of Arts Board of Trustees, and on the Homeless Services Advisory Committee. A life of service and commitment to the community and to humankind is the most fulfilling thing any person could wish. Dr. Burch is the Board Chair for FCR (Families and Communities Rising), Member of the Access to Care Committee, a Member of the National Kidney Foundation, Member of Red Mt. Lodge of the Prince Hall Masons, Durham Consistory #218, ZAFA Temple Shriners #176, and many other civic organizations.
Erika Cotrell, PhD, MPP
Dr. Erika Cottrell is Senior Investigator and Program Director of Research Networks at OCHIN. She also holds an appointment as an Associate Professor in the Department of Medical Informatics and Clinical Epidemiology at Oregon Health & Science University (OHSU). Trained as a sociologist with expertise in qualitative and quantitative methods, Erika has a robust research portfolio focused on community-based health centers, health policy, social and structural drivers of health, maternal and child health, and patient health experiences.
Since joining the OCHIN research department in 2013, she has led studies funded by the Agency for Healthcare Research and Quality (AHRQ), National Institutes of Health (NIH), Patient Centered Outcomes Research (PCORI), and Robert Wood Johnson Foundation (RWJF). Her research focuses on the impact of state and federal policy changes on provision of comprehensive preventive, prenatal, and postpartum care community health centers; the feasibility of using community- and individual-level social drivers of health data to inform decisions about health care performance and payment; developing and testing electronic health record (EHR)-based tools for integrating social risk screening and action into primary care; and understanding people’s experiences of opioid use disorder and treatment.
Currently, she is principal investigator (PI) of Accelerating Data Value across a National Community Health Center Network (ADVANCE), one of eight clinical research networks (CRNs) in the National Patient-Centered Clinical Research Network (PCORnet); multiple principal investigator (MPI) on the Network for Community-Engaged Primary Care Research (NCPCR), funded by NIH; and director of health experiences research for the Oregon Clinical & Translational Research Institute (OCTRI) at OHSU, which works to elevate patient voices in clinical and translational research.
Vanessa Marshall, Ph.D.
Vanessa Marshall is a Social Behavioral Scientist Administrator (Program Officer) in the Office of the Director at NIMHD. She manages and conducts research to advance public health prevention science. Her research focuses on improving health outcomes and promoting research to understand and address the multilevel determinants of factors that play a role in differences in health outcomes. She provides expertise in key research areas, including health services research, community engaged research, clinical trials, public health, quality improvement, implementation, dissemination, and evaluation. She has fostered innovative collaborations and partnerships to promote and support evidence-based research to inform clinical practice and policy. Dr. Marshall’s experiences have allowed her to work at local, regional, national, and international levels to investigate differences in health status and risk factors among communities to address health outcomes.
Prior to joining NIMHD, she worked at the U.S. Department of Veterans Affairs, Case Comprehensive Cancer Center, University Hospitals Cleveland Medical Center, Cleveland Clinic, and Howard University School of Medicine. Dr. Marshall has held federal, academic, clinical instructor, research scientist, and training coordinator positions, providing leadership and subject-matter expertise. She has organized and conducted numerous public health initiatives designed to promote and advance prevention, including those that engage patients through various screening programs and improve access to care. She has conducted research and evaluation projects across the lifespan of various communities and in the fields of infectious diseases and chronic diseases. She has served and volunteered on many community advisory boards, committees, professional organizations, and agencies. Dr. Marshall received her Ph.D. in public health from Kent State University, Kent, Ohio.
Sonja R. Fuqua, Ph.D., R.N.
Sonja R. Fuqua is the Chief Clinical Services Officer for the Community Health Center Association of Mississippi. With over 30 years in nursing, her experiences range from Obstetric nursing (clinical) to Manager of Research and Recruitment with the Jackson Heart Study (10 years), to four years with G. A. Carmichael Family Health Center (GACFHC), one of the CHCAMS member Community Health Centers. While with GACFHC, she served as the Patient-Centered Medical Home (PCMH) Director and was responsible for overseeing the organization’s readiness for PCMH recognition and completing the application process for which Level 2 recognition was achieved.
The study is being conducted through funding by the National Institutes of Health (NIH) National Heart, Lung and Blood Institute (NHLBI) and the National Institute on Minority Health and Health Disparities (NIMHD) (sub-OTA 6793-02-S027).
